Coronary Artery Bypass Grafting, commonly known as CABG (pronounced “cabbage”), is a surgical procedure to restore blood flow to the heart in patients with severe coronary artery disease (CAD). This comprehensive guide will cover all essential aspects of CABG, from why it’s needed to what you can expect before, during, and after the surgery. We’ll break down the information for general understanding, and then delve into medical specifics for healthcare professionals.
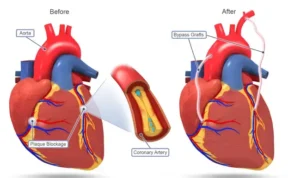
Coronary Artery Bypass Grafting (CABG) is a heart surgery that aims to improve blood flow to your heart. When the blood vessels that supply your heart (called coronary arteries) are blocked or narrowed, it can prevent enough oxygen from reaching the heart muscle, leading to chest pain, shortness of breath, and even heart attacks. CABG creates a new pathway (bypass) using a blood vessel taken from another part of your body, allowing blood to flow around the blockage and reach the heart.
Coronary Artery Bypass Grafting (CABG) is a revascularization procedure used to treat obstructive coronary artery disease (CAD), particularly in cases where percutaneous coronary intervention (PCI) is not viable or has failed. The procedure involves anastomosis of a graft vessel, such as the internal mammary artery (IMA) or saphenous vein graft (SVG), to the coronary artery distal to the occlusion, restoring myocardial perfusion.
CABG is recommended when the coronary arteries are significantly blocked, and other treatments, like medication or stenting, aren’t enough to improve blood flow. It’s commonly needed if:
Indications for CABG include:
If you have persistent chest pain, shortness of breath, or if you’ve been diagnosed with coronary artery disease, consult a doctor. They may conduct tests like an EKG, stress test, or angiogram to assess the severity of your condition and recommend CABG if needed.
The CABG procedure typically involves: