Cirrhosis is the late-stage consequence of chronic liver damage, where healthy liver tissue is replaced by scar tissue (fibrosis), leading to a permanent loss of liver function. It’s a serious condition that can result from untreated fatty liver disease, hepatitis, excessive alcohol consumption, or other chronic liver conditions.
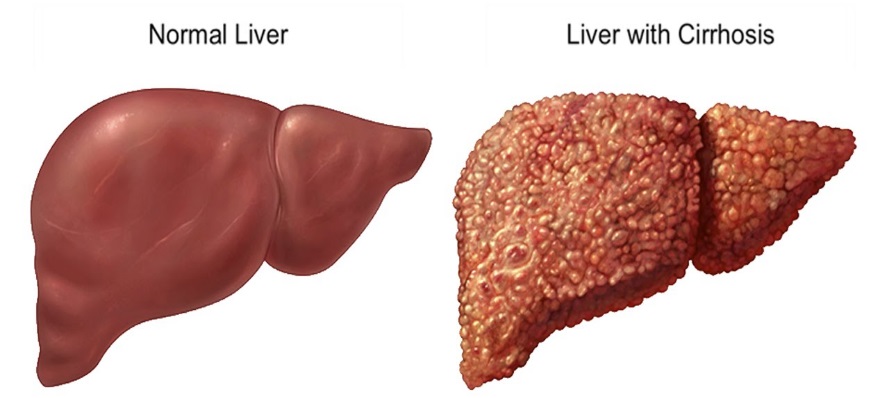
Cirrhosis is the late-stage consequence of chronic liver damage, where healthy liver tissue is replaced by scar tissue (fibrosis), leading to a permanent loss of liver function. It’s a serious condition that can result from untreated fatty liver disease, hepatitis, excessive alcohol consumption, or other chronic liver conditions.
Scar Tissue Formation:
Loss of Liver Function:
Cirrhosis often remains asymptomatic in its early stages, but as the liver becomes more damaged, symptoms appear:
Address the Underlying Cause:
Lifestyle Changes:
Medications:
Regular Monitoring:
Liver Transplant:
Preventing Cirrhosis
The best way to prevent cirrhosis is to treat liver problems early and maintain a healthy lifestyle:
Cirrhosis is a serious condition, but it is often preventable and manageable if caught early. Your liver is a resilient organ, capable of repairing itself if given the chance. If you’re experiencing any symptoms of liver trouble or have risk factors for liver disease, don’t delay—consult a healthcare professional to take action and protect your liver health.